It may surprise many people to know that dementia is not a normal part of aging. Dementia is a syndrome caused by a variety of brain illnesses that affect memory, thinking, behavior and the ability to perform everyday activities. It is true that memory declines in older adults, but normal memory problems should not affect everyday life. For example, misplacing a pen is very different from forgetting what a pen is used for.

Types of Dementias
Alzheimer’s
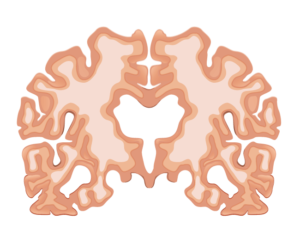
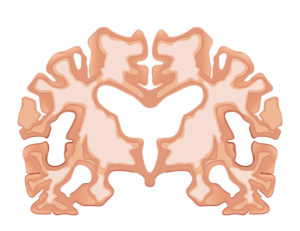
Alzheimer’s, a degenerative brain disease, is the most common form of dementia. Dementia itself is not a specific disease. The word is a general term for loss of memory and other mental abilities that are significant enough to interfere with everyday life. While Alzheimer’s represents 60 to 80% of diagnosed cases, there are many types of dementia–and all result from physical changes in the brain.