What is Oxygen Therapy?
To receive oxygen therapy means using supplemental oxygen to help increase your oxygen saturation, which is the amount of oxygen in your blood. The COPD foundation explains that the air we breathe typically contains 21% oxygen. Supplemental oxygen increases the oxygen levels we inhale when injury or illness cause the oxygen saturation in your blood to drop too low. According to the Mayo Clinic, the additional oxygen can help with healing. Some types of oxygen therapy, such as hyperbaric, may need to be administered in a hospital or clinical setting, while other forms can be administered at home, or even as you set off on your next adventure.
Normal Blood Oxygen Level
The amount of oxygen in your blood should be above 90%. However, healthy individuals without lung disease usually have oxygen levels greater than 95%. In cases where your oxygen saturation drops below 90%–92% you should see your doctor to determine if you need supplemental oxygen therapy. Blood oxygen saturation levels can be measured in a few ways, most commonly with a pulse oximeter.
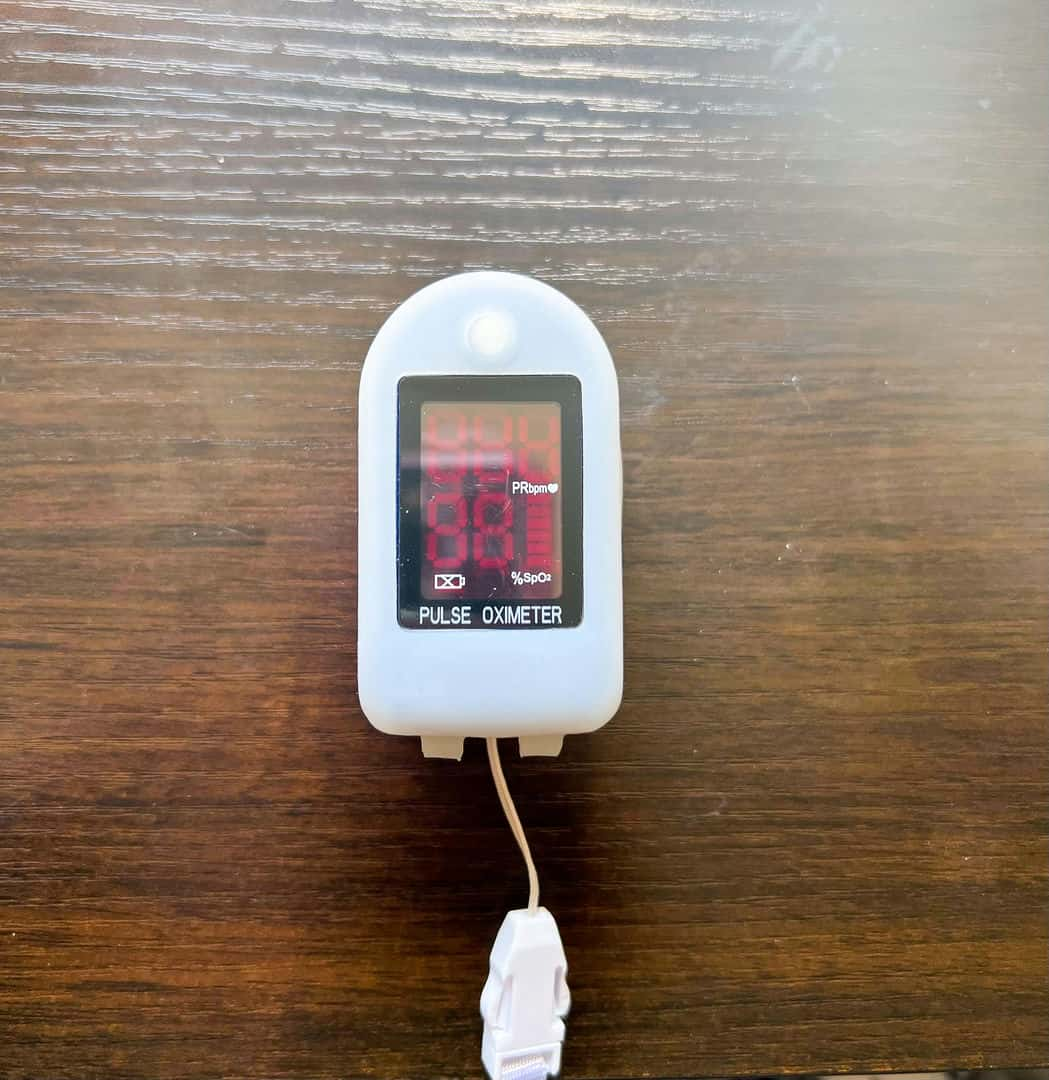
Pulse oximeter
A pulse oximeter is a small device that is placed on the fingertip and uses light to measure your oxygen saturation. This device is inexpensive and noninvasive and provides an immediate result. Medical professionals and home users rely on it to quickly assess the level of oxygen in the blood. Despite its benefits, there are some factors that can reduce the accuracy of the reading such as tobacco use, nail polish, artificial nails, and poor circulation, as well as the temperature, thickness, and pigmentation of your skin.
Arterial Blood Gas (ABG) test
“An ABG is very specific and ordered when CO2 and PaO2 (a measurement of oxygen pressure in arterial blood) are needed to determine actual measurements of lung function,” said Elizabeth Lyda, a licensed respiratory therapist and research quality improvement specialist at University of Rochester Medical Center. “These blood samples are drawn from an artery versus a vein, using a different technique and are much more painful than a regular blood draw.” The results of this blood test allow your doctor to determine how much oxygen is in your blood and how well you are releasing carbon dioxide. While it takes longer, and requires a blood draw, this test is more accurate.
Walk test
This test also uses the pulse oximeter, which you wear while walking on a treadmill or flat surface. This test will allow the doctor to measure how your body manages oxygen when your activity rate is increasing. If your oxygen saturation drops lower than it was when you started at rest, you may need supplemental oxygen during ambulation (walking) or exercise only.
Who Needs Oxygen Therapy?
Oxygen therapy can be helpful in both short-term and long-term situations. An example of a short term application of oxygen therapy would be a medic providing oxygen to someone who inhaled smoke during a fire. In most cases, they would only need the oxygen for a short amount of time and can return to normal activities with no long-term impact.
Long-term oxygen therapy is often in response to a chronic illness or injury that is progressive or taking a long time to heal. Some conditions that may require oxygen therapy include:
- Asthma
- Bronchitis
- Chronic obstructive pulmonary disease (COPD)
- COVID-19
- Cystic fibrosis
- Heart failure
- Lung cancer
- Lung disease
- Pneumonia
- Pulmonary fibrosis
- Pulmonary hypertension
- Sleep apnea
- Trauma to the respiratory system
- Low oxygen saturation not caused by one of the conditions above
Low Blood Oxygen Level
When an individual has low blood oxygen they have what’s called hypoxemia, and it can cause a number of health issues, leading to:
Difficulty exercising
Low blood oxygen can make exercising and other activities more difficult, ultimately weakening your muscles. When your oxygen saturation is low, your lungs are already working harder to get more oxygen into your system. Exercise requires effective oxygen saturation throughout your body. Your lungs and heart must be adequately oxygenated in order to oxygenate your blood and pump it to your other organs and muscles, and this need increases the more your muscles are used.
More red blood cells
Red blood cells transport oxygen to the body. When oxygen levels are low, the body makes more red blood cells in an attempt to transport more oxygen. These extra red blood cells can raise your blood pressure and cause headaches and blood clots.
Weaker heart
Low oxygen levels cause the heart to beat harder so it can spread oxygen throughout the body, which can weaken the heart over time, increasing the risk of heart failure.
Confusion and brain damage
Inadequate oxygen levels can cause confusion, as well as attention, memory, and speech problems, and in extreme situations, can result in damaged tissue in the brain and lead to coma and even death. These results vary widely based on how low your oxygen level gets and the amount of time it is low. While mildly lowered oxygen levels can impact your attention span and thought processes, many people endure this for long periods of time, and may not even be aware their oxygen is low. Extreme drops in oxygen can lead to brain damage and death in a short amount of time. Brain death occurs after 10 minutes without oxygen.
Symptoms of Low Oxygen Levels
You may have had a pulse oximeter clipped on your finger during some medical appointments. This quick reading is often done while they check your blood pressure. Low oxygen can be indicative of many different conditions, including age or being out of shape. According to the National Heart, Lung, and Blood Institute, many people with early stage COPD don’t even know they have it. COPD or chronic obstructive pulmonary disease, is a condition where obstructed airways make breathing difficult. Common examples of COPD are emphysema and bronchitis. Symptoms of low oxygen include:
- Shortness of breath
- Headaches
- Restlessness
- Dizziness
- Rapid breathing
- Chest pain
- Confusion
- High blood pressure
- Lack of coordination
- Visual disorders
- Sense of euphoria
- Rapid heartbeat
Types of Oxygen Therapy
Supplemental oxygen therapy can be delivered in several different ways. The type of oxygen treatment you receive will depend on a number of factors such as how much oxygen you need, whether you will need it both day and night, where you live, how active you are, and what your insurance will cover.
Oxygen gas cylinders
Cylinders of compressed oxygen are available in both small and large sizes. The smaller cylinders come in a variety of sizes, ranging from 8 pounds to just a few ounces and are often used as portable oxygen for activities away from the home. These cylinders will run out of oxygen quickly and must be handled with care as they can become dangerous if they fall. “Using cylinders is the standard setup for home oxygen and is still the most common way to provide portable oxygen,” said Lyda. “Regulators can be provided to ‘conserve’ tank life.”
Liquid oxygen
Oxygen becomes liquid when it’s supercooled (300 degrees Fahrenheit). It can then be stored in metal tanks that can provide oxygen without needing electricity. Home liquid oxygen delivery systems are quite heavy, as much as 120 pounds, but smaller, portable oxygen tanks can be filled from the large base tank. If you’re traveling, you will need to make arrangements for a large tank at each destination and ensure you have enough oxygen supply in your portable tanks to cover your traveling time. The large tanks must be refilled regularly at considerable expense, and up to a pound of liquid oxygen may evaporate per day. There is also the risk of frostbite if the liquid oxygen isn’t handled carefully when filling the tanks. This type of home oxygen therapy isn’t used often, and it’s not always available from providers in some parts of the country.
Oxygen concentrators
Oxygen concentrators pull oxygen directly from the air in the room so there’s no need for a tank or refills. The home oxygen concentrator uses electrical pumps, so it must be plugged into an outlet or a battery. The home unit is usually on wheels and weighs 30–50 pounds, while portable oxygen concentrators (POCs) range in weight from 3–20 pounds. These lightweight units are often referred to as ambulatory oxygen concentrators, highlighting the ease with which they can be carried around.
Because you don’t have to make any special arrangements for tank delivery, POCs are well-suited for traveling. It’s also the only type of oxygen therapy that is currently permitted on commercial airlines. Oxygen concentrators provide 85%–95% oxygen, which may not be a high enough concentration for some people, so it’s not ideal for everyone.
Hyperbaric oxygen therapy
Hyperbaric oxygen therapy is administered in a hospital or clinical setting. It takes place in a chamber, which uses 100% pure oxygen, where the air pressure is two to three times higher than normal. This higher pressure allows your lungs to oxygenate your blood at a higher rate.
This type of oxygen therapy treats much more than lung issues. The higher oxygen levels in the blood can help heal a wide range of injuries and illnesses, including:
- Brain abscess
- Bubbles of air in your blood vessels (arterial gas embolism)
- Burns
- Carbon monoxide poisoning
- Crushing injury
- Decompression sickness
- Exceptional blood loss anemia
- Gangrene
- Infection of skin or bone that causes tissue death
- Non-healing wounds
- Radiation injury
- Skin graft or skin flap at risk of tissue death
- Traumatic brain injury
Hyperbaric oxygen therapy is not without risk. Although rare, the higher pressure and oxygen concentration can cause some side effects, like:
- Middle-ear injuries
- Temporary nearsightedness
- Lung collapse
- Seizures as a result of too much oxygen (oxygen toxicity)
- Lowered blood sugar in people with insulin-treated diabetes
Transtracheal oxygen therapy
If you have a hard time with the nasal cannula (the device that delivers the oxygen to your nose), a mouth or throat injury, or need higher levels of oxygen, your doctor might recommend transtracheal oxygen therapy. Dr. Ordessia Charran, a pulmonologist with Kingman Pulmonary Associates, explained the process. “In general, a very select patient population may require oxygen delivered directly via the trachea. It is not commonly recommended in the vast majority of people since it involves a surgical procedure and having a foreign body implanted in your trachea.”
In this process, a small hole is placed in your neck and trachea, and a breathing tube is placed in the hole. The oxygen treatment can then be applied directly to the breathing tube in your neck rather than through your nose. It may take some practice, and the help of a speech therapist, to regain your ability to speak and swallow because the catheter is placed below the vocal cords. Other complications are quite rare, but include bleeding, infection, collapsed lung, scarring, air trapped under the skin, and fistula (an undesired connection between your trachea and esophagus).
Oxygen Therapy Equipment
Oxygen therapy involves specialized equipment, whether you’re receiving the treatment in a hospital or at home. If you’re receiving this treatment at home, your health care provider will connect you with a local durable medical equipment (DME) supplier who will bring the oxygen tanks or concentrator to your home. They will also be your supplier for portable tanks and concentrators and all the accessories needed to use oxygen equipment, which include:
Nasal cannula
This has two hollow prongs to go in each nostril and connects to the tubing to deliver the oxygen directly to your nose. The cannula should be wiped clean each day and replaced each month.
Tubing
This is the hose that delivers the oxygen from your tank or concentrator to the nasal cannula or face mask. The tubing should be replaced every six months. High-flow oxygen (more than 6 liters per minute) will require special tubing.
Face mask
The face mask is used with high-flow oxygen therapy. It covers both the nose and mouth and connects to the tubing to provide you with oxygen. The face mask should be cleaned once or twice a day and replaced monthly. “[High flow oxygen therapy is] rarely used with an oxygen concentrator as there is not enough flow produced, and back pressure can turn the concentrator off,” said Lyda.
Humidifier
Oxygen therapy can dry out your nasal membranes. The humidifier is attached to the oxygen therapy system and mixes distilled water with the oxygen. Humidifiers are not to be used with portable oxygen therapy devices.
Filter
Filters keep unwanted particles such as dust or bacteria out of your oxygen. The type of filters you will need will vary with the make and model of your oxygen therapy device.
Pulse oxygen delivery device
Also known as an oxygen conserving device (OCD), this device helps to reduce the amount of oxygen used by only delivering oxygen when you inhale. It senses the start of your inhalation and provides a pulse of oxygen with it. You must inhale strongly enough for the sensor to detect it, so your doctor will test your ability to maintain sufficient oxygen saturation while using this device. Some people may not have the strength in their inhale to trigger the pulse, so they would be better served by a continuous-flow system than the pulse flow.
Oxygen Therapy Benefits
It’s easy to grow accustomed to the symptoms of low blood oxygen. Over time, the headaches, shortness of breath, and racing pulse may start to feel like the symptoms of age. However, those symptoms can often be reduced or eliminated. There are benefits to oxygen therapy. It can make you feel better, and portable oxygen therapy options allow you to continue with many of your favorite activities.
More energy
Low oxygen levels cause fatigue when your muscles don’t have enough oxygen to power them. The increased oxygen will give you the energy to be more active and get back to those activities you enjoy. More activity will help you live a healthier and more vibrant life.
Better sleep
When your oxygen levels drop during sleep, it can cause you to wake frequently and sleep fitfully. Oxygen therapy can help you maintain healthy oxygen levels while you sleep, and a more productive sleep will help you feel better the next day.
Increased survival
The COPD Foundation explains that using oxygen therapy may help you live longer and feel better at the same time. By reducing the symptoms and effects of low oxygen, your body can become healthier, and you can get back to your favorite activities.
Fewer symptoms of COPD
COPD conditions such as bronchitis and emphysema can cause breathlessness, fatigue, dizziness, and swollen ankles. Oxygen therapy helps stabilize your oxygen levels and reduce these symptoms.
Improved quality of life
Improved oxygen levels will help you feel better, get better sleep, and have more energy whether you’re receiving the oxygen at the hospital, in your home, or on the go. With a portable oxygen concentrator or tank, you can go out with friends, have adventures, and feel good doing the things you love to do.
What are the Side Effects of Being on Oxygen?
Irritation of the skin and nasal passages
This is the most common side effect of oxygen therapy. The tubes and cannula rubbing against the skin can lead to irritation, and the oxygen can cause the nasal passages to dry out. A water-based moisturizer can help soothe the skin and moisten the nasal passages.
Oxygen toxicity
Oxygen toxicity most often occurs in divers, infants in incubators, and those receiving hyperbaric oxygen treatment. It can also occur when patients try to increase their oxygen levels above what was prescribed. “Oxygen toxicity occurs when patients use supplemental oxygen to achieve an oxygen saturation that is too high for their current lung disease or condition,” said Dr. Charran. “It is often seen in patients with COPD who feel short of breath and increase the amount of oxygen their device delivers to achieve an O2 saturation of less than 92%.”
For certain individuals, too much supplemental oxygen can damage the lungs and other organs. It’s important that you don’t increase the flow of oxygen to try to increase your oxygen saturation above 92%. Target oxygen saturation for therapy should be 88%–92% rather than 100% to help protect against oxygen toxicity. “In general, we do not recommend using supplemental oxygen to get your saturation up to 100%,” said Dr. Charran. “Again, it is safest to ask your health care provider what your desired oxygen saturation range is and stick to it!”
Safety Considerations
Oxygen therapy comes with some risks that can be reduced if care is taken and safety is prioritized. The American Lung Association provides guidelines on oxygen safety.
This list of safety considerations should be taken seriously and shared with caretakers, family, and friends:
- Petroleum- or paraffin-based lotions and lip balms can burn in an oxygen-rich environment. Be sure to use water based moisturizers while using oxygen therapy.
- Do not smoke or allow others to smoke near you while you are using oxygen therapy because the supplemental oxygen increases the risk of fire and supports combustion.
- Avoid flames such as candles, bonfires, gas stoves, pilot lights, and fireplaces. Stay at least 6 feet away from any spark of flame.
- Do not use electrical appliances that can cause a spark, including electric razors and hair dryers.
- Place a sign in the front of your home to notify visitors you are using oxygen.
- Inform your fire department and local power company that you are using oxygen therapy in your home. The fire department needs to know that your home is at higher risk for fire because of the oxygen enriched environment. This is for your safety and that of their firefighters. If the power company is aware that you’re using an oxygen concentrator dependent on electricity, they can flag your home for priority restoration in case of a power outage.
- Keep fire extinguishers in your home. Maintain fresh batteries in your smoke detector.
- Pressurized oxygen cylinders will propel like torpedoes if they crack, so take care to keep them from falling. Large cylinders should be secured in place. Small cylinders should be handled with care.
- Do not try to repair your oxygen therapy system yourself. Contact your DME supplier if something needs to be fixed. Contact them immediately if you notice a crack in your oxygen tank.


